Pediatric joint hypermobility: a diagnostic framework and narrative review - summary
- Kirstin Maltby
- May 6, 2023
- 3 min read
A new article (click here) has been published thats focuses on the diagnostic criteria of paediatric joint hypermobility. They have thankfully made this an open article so we can read it fully.
The Paediatric Working Group Have been meeting regularly between 2020-22 and have an assortment of international* health professionals who work with hypermobility. 5000 paediatric patients were assessed and substantial reviews of peer-reviewed articles was conducted in coming up with the paediatric framework.
The article starts by highlighting that the diagnosis of hypermobile Ehlers-Danlos (hEDS) and hypermobile spectrum disorders (HSD) are clinical due to a lack of known genetic markers and mainly made for adults; this makes the diagnosis for kids difficult due to their inherent hypermobility and they may not be old enough to develop some criteria (stretch marks etc). As there are so many comorbid conditions and early intervention is essential for better outcomes they highlight the imperative need for a review of pediatiec diagnosis. The current diagnostic criteria for hEDS is the 2017 criteria for hypermobile Ehlers–Danlos syndrome
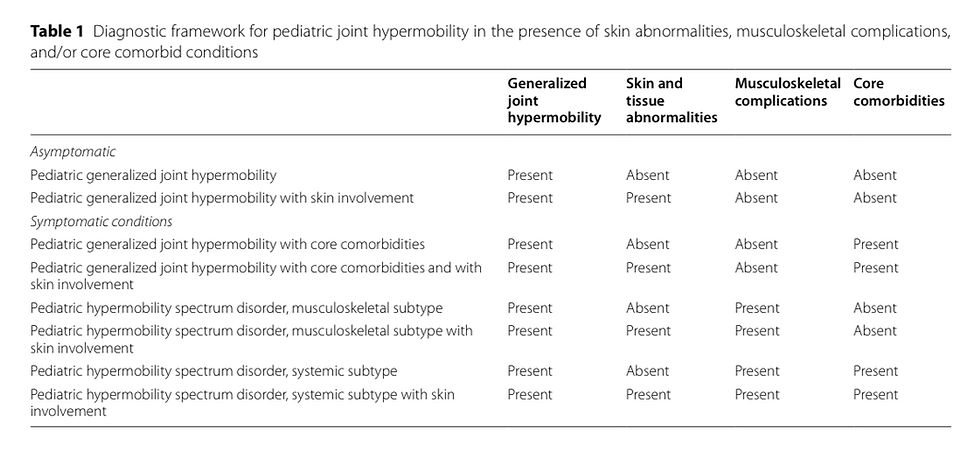
A framework of four components looking at generalised joint hypermobility, skin and tissue abnormalities, musculoskeletal complications and core Comorbidities. The framework is supposed to be fluid so a child may change within the framework and later may achieve and EDS diagnosis when they reach maturity.
The subtypes suggested are listed on the table below.
The framework has four main categories, with or without skin involvement which then yields eight in total a child may fit in. It is also not recommended that children who fit any of these criteria undergo genetic testing right now due to the lack of genetic bio markers available. There are 4 criteria ecg with individual scoring and a minimum required in each section. It is suggested this done AFTER other types of EDS are excluded. A minimum age of 5yrs is recommended as children below this age have insufficient bone maturity. The upper age limit is when a child reaches biological maturity, which is defined as skeletal maturity with growth velocity less than 1 cm/year using 2 measures at least 3 months apart, or a mature bone age x-ray. After this of when they have reached 18yrs of age they can be assessed under the 2017 hEDS criteria if still required.
Generalised Joint Hypermobility: due to children being generally "bendier" it's suggested a Beighton Score of 6 or more out of 9. They also recommend doing further tests if a positive Beighton Score is achieved for a more thorough assessment for identifying needs and a comprehensive musculoskeletal examination
Skin and Tissue Abnormalitles: soft skin, stretchy skin, atrophic scars, stretch marks, piezogenic papules, and recurrent hernias. The presence of scarring and stretch marks at 3yrs was considered a greater predictor of disability compared to soft and stretchy skin.
3 out of 5 skin features needed to be present to meet criteria
hEDS is reserved for biologically mature adolescents who meet the 2017 criteria, which also covers even rarer types of Ehlers–Danlos syndrome at any age. It is not recommended
Musculoskeletal episodic, activity related pain: Adolescents generally have a higher level of instability in areas like the patella. Soft tissue injuries were also a common feature found in patients who were diagnosed with EDS.
Children when they reach maturity (around 18) can be reassessed if they generalise hypermobility remains a problem for a potential EDS diagnosis.
Core Comorbidities: one thing EDS is well known for is the amount of comorbidities that seem to occurs with some recent literature showing issues like POTS occurring at a rate of 88% and MCAS at a rate of in 81% EDS patients. This is a challenge however as some features like widespread musculoskeletal pain is a common finding in comorbid disoededs like Dysautonomia. Even though the presence or absence of any of these disorders does not influence diagnosis they impact the different subtypes in the framework. The list of potential comorbid includes
• Chronic Pain
• Chronic Fatigue
• Functional Gastrointestinal Disorders
• Functional Bladder Disorders
• Anxiety
There are some emerging Comorbidities not yet listed but may be included in the future with more research: inflammatory arthritis, developmental coordination disorders, autism spectrum disorders, attention deficit hyperactivity disorder, idiopathic scoliosis and Menorrhagia and dysmenorrhea.
*One a side note we have an Australian to thank for their contribution in this article - Louise Jane Tofts. We will be updating our website accordingly in the next few weeks.
References:
Images were from the article which is free to view.
Beighton Scale: https://www.ehlers-danlos.com/assessing-joint-hypermobility/






Our expert, unbiased review of Gransino Casino reveals a feature-rich platform. The welcome bonus is solid, and ongoing promotions add value. Its game library is huge, with everything from pokies to a full https://gransino.co.com/ sportsbook. We verified its payment methods, which are secure and efficient. Gransino’s established reputation makes it a reliable choice. Count on us for a truthful assessment.